Symptoms
The main symptoms are abnormal bleeding:
- Bleeding after the menopause
- Bleeding between periods
- Bleeding that is unusually heavy
- Blood stained discharge – from light to dark brown
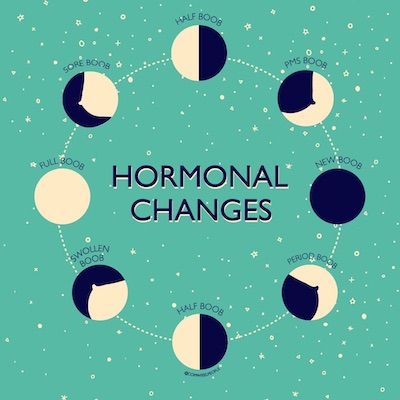
If you have ovaries, you may still have monthly bleeding with your cycle. If you are taking testosterone, it is likely you may have a change in periods or they may stop completely. Every person is different and bodies react differently to hormones. It is important to know your normal, and if anything changes, speak to a doctor.
Risk factors
Obesity
Obesity can increase the risk of womb cancer by tenfold, as fat cells produce oestrogen. Oestrogen, if not balanced by a second reproductive hormone, progesterone, can lead to abnormal growth of the cells lining the womb and increase the risk of cancer, so the risk remains even if you have had your ovaries removed.
Testosterone
There is currently not much research out there around the effects of testosterone on gynaecological cancer risk. Some studies have indicated that if you have been taking testosterone and have a womb, you may have an increased risk of womb cancer due to the effect of testosterone on the womb lining (endometrium). The current recommendation is for trans men and non-binary people who have a womb and have been taking testosterone for more than two years, to have a pelvic ultrasound every two years.
Hereditary cancer risk
A very small percentage of people develop womb cancer because of an inherited genetic condition called Lynch Syndrome. If one of your immediate family members knows they have Lynch syndrome you will be eligible for testing. You should also consider being tested if several members of your family have suffered from bowel, womb or breast cancer. You can find out more about Lynch Syndrome here.
Content provided by The Eve Appeal
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers – womb, ovarian, cervical, vulval and vaginal.

Published on Wed, 09 Mar 2022 12:35:20 GMT
Modified on Mon, 21 Mar 2022 10:21:40 GMT
Symptoms:
- Increased abdominal size and persistent bloating (not bloating that comes and goes)
- Persistent pelvic and abdominal pain
- Unexplained change in bowel habits
Difficulty eating and feeling full quickly, or feeling nauseous
Risk factors:
Family history
If you have two or more close relatives who developed ovarian cancer or breast cancer, your risk of also developing the condition may be increased.
If your relatives developed cancer before the age of 50, it’s more likely it was the result of an inherited faulty gene. BRCA1 and BRCA2 are genes that when altered are linked to ovarian cancer, breast cancer, prostate and pancreatic cancers.
You may be at a high risk of having a faulty gene if you have:
- One relative diagnosed with ovarian cancer at any age and at least two close relatives with breast cancer whose average age is under 60; or alternatively at least one close relative with breast cancer under the age of 50. All of these relatives should be on the same side of your family (either your mother’s OR father’s side)
- Two relatives from the same side of the family diagnosed with ovarian cancer at any age.
If you’re at a higher risk of having the BRCA gene alteration, your GP can refer you for tests to check for faulty BRCA1 and BRCA2 genes.
Hormones
If you are on hormone treatment, it may alter your risk. There is a small reduction in risk if you are on or have taken a combined contraceptive pill. There may be a slight increase in risk on certain types of HRT. There is currently very little research into the effects of testosterone on ovarian cancer risk.
Content provided by The Eve Appeal
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers – womb, ovarian, cervical, vulval and vaginal.

Published on Wed, 09 Mar 2022 12:42:43 GMT
Modified on Mon, 21 Mar 2022 10:21:57 GMT
This may be relevant to you if have not had a total hysterectomy (removal of the womb and cervix).
Most cervical cancers are caused by a common sexually transmitted infection called human papillomavirus (HPV). HPV is a group of viruses, of which there are more than 100 different types and are responsible for skin warts, genital warts and verrucae. A number of these viruses , known as High Risk HPV can infect the cervix and cause no visible symptoms If the body is unable to clear High Risk HPV, there is a risk of abnormal cells developing, which could become cancerous over time. High Risk HPV is spread during sexual skin-to-skin contact, which is why it is important to get vaccinated if applicable, and go for your cervical screening, if applicable, even if you have not had penetrative sex. The UK government offers a HPV vaccination to all children at 11-12 years old.
It is currently the only gynaecological cancer with a national screening prevention programme, which is estimated to save around 4000 lives a year. In the UK, from the age of 25 everyone with a cervix is eligible for screening every 3-5 years, depending on their age. You can find out more about screening HERE.
Symptoms:
- Abnormal bleeding
- Bleeding between periods
- Bleeding after penetrative sex
- Bleeding that is unusually heavy
- Discharge – unpleasant smelling or blood stained
- Bleeding after the menopause
- Pain
Risk factors:
Smoking
People who smoke are twice as likely to develop cervical cancer as those who don’t; this may be caused by the harmful effects of chemicals found in tobacco on the cells, which make the immune system less effective, and less able to clear the HPV virus from your body and more vulnerable to the effects of the virus.
Immunosuppression drugs
People who are on immunosuppression drugs long term (organ transplant recipients), can be at increased risk of retaining the HPV virus and developing cervical cancer.
Further information about cervical screening for trans men, non-binary and intersex people is available.
Content provided by The Eve Appeal
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers – womb, ovarian, cervical, vulval and vaginal.

Published on Wed, 09 Mar 2022 14:29:58 GMT
Modified on Mon, 21 Mar 2022 10:23:44 GMT
This is relevant to you if you’ve not undergone genital surgery, or if you’ve had a phalloplasty or a metoidioplasty (both sometimes referred to as bottom surgery), as part or all of the vulva is kept and remodelled. The vulva describes the external genitals, including the soft tissue (labia minora and labia majora), the clitoris, and the Bartholin’s glands.
Symptoms:
- A lasting itch on the external genitalia
- Pain or soreness on the external genitalia
- Thickened, raised, red, white or dark patches on the skin of the external genitalia
- An open sore or growth visible on the genital skin
- A mole on the external genitalia that changes shape or colour
- A lump or swelling on the external genitalia
All these symptoms can be caused by other more common conditions, such as infection, but if you have any of these, you should see your GP. It is unlikely that your symptoms are caused by a serious problem but it is important to be checked out… remember non- cancerous conditions can be uncomfortable and so much better when treated!
Risk Factors:
Skin conditions that cause inflammation may sometimes develop into an early cancer. The two most common of these being vulval intraepithelial neoplasia (VIN) and Lichen Sclerosus. Some of these cell changes will go away without the need for any treatment; however, finding these abnormal cells early can help to prevent cancer.
Smoking
Smoking increases your risk of developing VIN and vulval cancer. This may be because smoking makes the immune system less effective, and less able to clear the HPV virus from your body and more vulnerable to the effects of the virus.
Vulval intraepithelial neoplasia (VIN)
VIN is potentially a pre-cancerous condition. This means there are changes to certain cells that aren’t cancerous, but could become a cancer at a later date if left untreated. This is a gradual process that usually takes well over 10 years.
There are two types of VIN:
- Usual or undifferentiated VIN – this typically affects people under 50 and is thought to be caused by an HPV infection
- Differentiated VIN (dVIN) – this is a rarer type, usually affecting people over 60, associated with skin conditions that affect the area, and is more likely to be associated with cancer.
Human papilloma virus (HPV)
HPV is present in at least 40% of cases, which suggests it may increase your risk of developing the condition. HPV is known to cause changes in the cells, which is known as VIN.
Content provided by The Eve Appeal
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers – womb, ovarian, cervical, vulval and vaginal.

Published on Wed, 09 Mar 2022 14:35:33 GMT
Modified on Wed, 09 Mar 2022 15:59:37 GMT
This is relevant to you if you’ve not undergone genital surgery, or some of your vaginal wall was remodelled during a metoidioplasty or if some vaginal tissues was left or remodelled during a phalloplasty procedure (both procedures are sometimes referred to as ‘bottom surgery’).
Symptoms:
- Abnormal bleeding, eg. between periods, after menopause
- Discharge with an unpleasant smell or blood stained
- Pain during penetrative sex
- An internal lump or growth that you or your doctor can feel
- An internal itch that won’t go away and pain when urinating
- Persistent pelvic and internal pain
Risk Factors:
Human papilloma virus
HPV is present in more than two-thirds of cases, which suggests that it may increase your risk of developing the condition.
Abnormal cells
Vaginal intraepithelial neoplasia (VAIN). VAIN is a term used to describe cells that are abnormal, which are thought of as a pre-cancerous condition. It is thought to be closely linked to having a persistent HPV infection. If left untreated it can turn into cancer.
Content provided by The Eve Appeal
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers – womb, ovarian, cervical, vulval and vaginal.

Published on Wed, 09 Mar 2022 14:37:49 GMT
Modified on Mon, 21 Mar 2022 10:23:52 GMT
Everyone with a cervix should be able to access the NHS cervical screening programme, and we want to provide helpful information for every community. Here we have answered some frequently asked questions:
When am I due to go for my first cervical screening?
Cervical screening (also known as a smear test) begins at the age of 25 in the UK. Around the time of your 25th birthday you may receive a letter inviting you to book your first screening appointment. If you are registered as male on your records, you will not get a letter asking you to book your appointment, but at the age of 25 you can contact your GP, or specialist clinic, and book your screening test.
You will be eligible for your next screening test every three years until the age of 50, and then every five years until the age of 64, if your screening tests are normal.
Although you will no longer receive screening invitations after the age of 64 as the risk of developing cervical cancer is low, you can still request cervical screening.
If you are 65 or over and feel you would benefit from a cervical screening appointment, please contact your GP.
What is a cervical screening test and how does it work?
The cervical screening programme is designed to protect against cervical cancer. This is because it can detect precancerous changes to the cells of the cervix, which if left untreated, could potentially develop into cervical cancer in the future. These changes give no symptoms which is why it is important to attend for screening. Please don’t be scared that this is a cancer test, it is designed to be preventative and reduce your risk.
The doctor or nurse will take a sample of cells from your cervix. They will do this by inserting a speculum (small plastic instrument) into the vagina, which holds the vaginal walls apart and allows the nurse or doctor to clearly see your cervix. They will then sweep the cervix with a soft plastic brush to collect the cells. Your sample will be sent to a laboratory for testing, where they will look first of all for high-risk HPV (human papillomavirus), a virus that causes almost all cervical cell changes. If high-risk HPV is present, your cells will then be tested for any abnormalities. It is important to remember that most people who have high-risk HPV will not have any cervical cell changes.
HPV is a common virus passed on through skin to skin sexual contact that causes over 99% of all cervical abnormalities. Your changes will be categorised into mild, moderate or severe dyskaryosis.
Will the cervical screening test hurt?
For some people, a cervical screening test can be uncomfortable. If you’re someone who doesn’t typically experience vaginal penetration, then there may be a higher chance of an internal examination causing you some discomfort.
If you are taking an oestrogen suppressant i.e. something that is stopping your ovaries from oestrogen, you will have less natural lubrication.
Using a natural vaginal moisturiser before your appointment will help to make the screening test more comfortable, and asking the doctor or nurse to use the smallest speculum can help minimise discomfort.
I’m a trans-man. Do I need to go for a cervical screening test?
Anyone with a cervix is at risk of developing cervical cancer. If you are a trans man who has a cervix, we understand that attending a cervical screening appointment may be emotionally and physically difficult for you. It can be helpful to have a separate appointment your nurse or doctor beforehand, and talk through the process with them. We have created a list of tips for helping with your screening, HERE. If you have any worries or concerns about going for your screening, do speak to your nurse, doctor or our Ask Eve information service.
I am a non-binary, do I need to go for a cervical screening test?
If you have a cervix, you will still be at risk of cervical cancer and we encourage you to attend your cervical screening appointment. This can understandably be something that is difficult to navigate, but your nurse and doctor are there to help you make the experience as positive as possible. Speak to them beforehand, go through what the appointment will involve and do check our list of tips on cervical screening, HERE. If you have any worries or concerns about going for your screening, do speak to your nurse, doctor or our Ask Eve information service.
I am intersex, do I need to go for a cervical screening test?
Not everyone who is intersex will need a cervical screening test. If you are intersex, it will depend on your combination of internal reproductive organs, i.e. whether or not you have a cervix, as to whether or not you need the screening test.
Your nurse or doctor will want to make you feel comfortable and reassured during this procedure, and good communication between the two of you is really important. Take your time, ask the questions you need answers to in order to feel as in control and relaxed as possible. Our tips on screening for trans men, non-binary and intersex people with a cervix can be found HERE, and our Ask Eve information service team are here to help you.
I have had the HPV vaccine, do I need my screening test?
Yes. The HPV vaccine available on the NHS works against four strains of HPV: 6, 11, 16 and 18. Types 16 and 18 cause around 70% of all cervical cancers. There are 11 other strains of high-risk HPV (HPV that can cause precancerous abnormalities) that are not currently included in the vaccination. It is still important to go for your screening test to pick up on any abnormal changes to your cervix. Together, the vaccination (typically given to children age 12-13) and screening programme in the UK prevent thousands of cases of cervical cancer a year. We encourage people to have both the vaccine and regular screening tests if applicable to you.
I haven’t had penetrative sex. Do I need to go for my screening test?
If you have never had penetrative sex, it is not a guarantee that you do not have any cervical abnormalities. Remember that sexual contact, without full intercourse can still transmit HPV. If you have never had any type of sexual contact then you are at a lower risk of cervical cancer, but as a small number of cervical cancers are not caused by HPV, so we would still recommend that you attend your screening appointment.
Jo’s Cervical Cancer Trust also has information and advice on their website which you might find helpful.
Content provided by The Eve Appeal
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers – womb, ovarian, cervical, vulval and vaginal.

Published on Wed, 09 Mar 2022 14:38:21 GMT
Modified on Mon, 21 Mar 2022 10:24:19 GMT
- Get booked in: if you’re registered as male at your GP surgery, you may not receive an invitation letter to go for your cervical screening. If you are 25 or over and have a cervix do call your GP and find out if you are due and get an appointment booked.
- Expectations: There is no pressure to actually have your screening test done in your first appointment. Sometimes multiple appointments are needed so that trust is built up between you and your nurse or doctor. If you are finding your screening difficult for whatever reason, it’s absolutely fine to need extra time in order to feel ready and prepared.
- Ask questions: Try not to be afraid to ask questions, or talk through any concerns you may have. Knowing what to expect can help make things seem less scary. It can be useful to see the equipment first and talk through the procedure step by step. If your nurse or doctor doesn’t ask for your pronouns, if you have had any genital gender transition surgeries or if you have a preferred term for your body parts, then try and tell them as early on in the appointment as possible, to avoid any communication that makes you feel triggered or uneasy.
- Start small: A speculum is the plastic instrument inserted in order to give the nurse or doctor a good view of the cervix. Speculums come in different sizes, so if you think you might find the screening test painful, ask for the smallest speculum and for it to be well lubricated.
- Ask Eve: Our nurse led information service, Ask Eve, is also here to help you. You can contact Ask Eve with any of your questions around gynae health and screening. You can email them on nurse@eveappeal.org.uk or call 0808 802 0019. The service is completely free and confidential, so please do get in touch if you want to talk to someone before (or after) your appointment.
- Relaxation is key: As humans, when we hear the words ‘just relax’, we often do the exact opposite! But try to relax in whatever way you can. What normally relaxes you? Whether it’s playing your favourite music or having a friend or partner with you for support, then use these tools to help you during your screening. Whatever you can do to try and feel as calm as possible. Control: Remember, you are in control of this situation! You can tell your nurse or doctor to stop and change your mind at any time for any reason.
- Lubricate: If you are post-menopausal or taking testosterone, you will have less natural lubrication, which can make a cervical screening test more uncomfortable. Try using a natural internal moisturiser before the appointment to make using a speculum easier and more comfortable. An oestrogen cream is also something that is helpful in this situation, but understandably using an oestrogen-based product can be off-putting, even if it is a localised product, i.e. won’t do anything to the body other than create more natural lubrication.
- You first: If you are finding the appointment really difficult, or taking the sample is causing a lot of discomfort or pain, it may be better for you to not go through with the screening test at this point in time. There might be a time in the future where it might be better for you. Sometimes, after thinking about your risk of having HPV, i.e. your sexual activity/history, you may decide against screening. Your overall wellbeing is a priority, particularly if the risk of cervical cancer is low. Your doctor or nurse will be able to discuss your risk with you and help you make the decision which is best for you and your overall health. You can also speak to Ask Eve.
- Plan B: If your GP/practice nurse finds it difficult to take your screening test, you can ask to be referred to your local colposcopy clinic where there is often a wider variety of equipment to make the process as comfortable as possible. There are some specialist LGBTQ+ clinics across the country too, which if possible, you can book into for your screening.
- Plan C: Sometimes it just isn’t possible to finish the test or you would prefer not to go ahead with the appointment. If you think it is a better option for you, you might want to consider a self-testing kit that can be done at home. It will come at a financial cost, and the chances of a poor sample or inaccurate result are higher, but it may be a better option if you would really like to be screened but are finding it too difficult.
If you still have any worries or concerns ahead of your appointment, you can contact our nurse-led information service, Ask Eve, by emailing nurse@eveappeal.org.uk, or calling the freephone number 0808 802 0019.
Content provided by The Eve Appeal
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers – womb, ovarian, cervical, vulval and vaginal.

Published on Wed, 09 Mar 2022 14:46:39 GMT
Modified on Mon, 21 Mar 2022 10:27:41 GMT
Preparation
- Make the offer: Trans men will not receive an invitation letter to go to a cervical screening so do keep in mind when seeing them whether they may need a screening test, make them aware they are due and chat them through what the test is and why they might want to have one.
- Don’t assume: If you don’t already know, check with your patients what their pronouns are. Check what gender reassignment genital surgeries your patient has had, if any. Also ask your patient what they prefer their genitals to be called, avoid words like vagina/vaginal unless told otherwise.
- Set expectations: Let your patient know that there is no pressure to actually have their screening done in your first appointment together. Sometimes multiple appointments are needed so that trust is built up and your patient can prepare themselves in whatever way they need to, before a sample can actually be collected from their cervix. Try to avoid language such as ‘successful’, ‘inadequate’ etc.
- Show and tell: Show your patient the equipment you will be using first. Knowing what to expect can help make things seem less scary. Show them the speculum and brush you plan to use and talk them through the procedure step by step before you begin.
- Be aware: that your patient may not have experienced any vaginal penetration, which includes vaginal intercourse, using sex toys or tampons. Therefore they may find a speculum painful. Try the smallest size speculum, and make sure it is lubricated.
- Relaxation is key: As humans, when we hear the words ‘just relax’, we often do the exact opposite! But if you can, let your patient know before your appointment together that being relaxed is important and will make the screening process easier. What normally relaxes them? Let them know they can bring in their favourite music, a stress ball, or a friend or partner for support. Whatever they can do to try and feel as calm as possible.
- Testosterone: may affect the results of a cervical screening test, so be sure to check with your patient whether or not they are currently taking testosterone. Testosterone can cause changes to the cervix that can mimic cervical dysplasia (abnormal cells). Using an extended brush can help to get a better sample of cervical cells. Someone taking testosterone is more likely to receive an abnormal cervical screening result, and be referred for a colposcopy. Let your patient know that this is the case and reassure them that taking testosterone isn’t increasing their risk of cervical cancer.
Performing the screen
1. Control: Throughout the appointment remind your patient that they are in control, and that they can tell you to stop or change their mind at any time. Some patients can feel very vulnerable during a screening appointment, so letting them know that everything is on their terms can help balance this. Letting them know that if it is easier for them they can help you guide in the speculum. Get informed and explicit consent, and double or triple check!
2. Moisture: If your patient is taking testosterone, they will have less natural vaginal lubrication, which can make a cervical screening test more uncomfortable for them and harder for you in terms of inserting the speculum. Advise them to use a natural vaginal moisturiser before the appointment to make using a speculum easier and more comfortable. An oestrogen cream is also something that is helpful in this situation, but understandably many trans men will not want to use anything oestrogen-based, even if it is a localised product, i.e. won’t do anything to the body other than make the vaginal wall more moisturised.
3. Patients first: If your patient is finding the appointment really difficult, or taking the sample is causing a lot of discomfort or pain, it may be better for your patient to not go through with the screening test at this moment. It might be better to recommend trying again at another appointment. Sometimes, after thinking about their risk of having HPV, i.e. their sexual activity/history (if any), a patient may decide against completing their screening. Their overall wellbeing is a priority, particularly if the risk of cervical cancer is low.
Follow up
4. Plan b: Sometimes it just isn’t possible to finish the cervical screening test, either because you can’t take the sample or your patient would prefer not to go ahead with the appointment. If appropriate, you might want to tell your patient about self-testing kits that can be done at home. It will come at a financial cost to them, and the chances of a poor sample or inaccurate result are higher, but is better than no test at all.
Dr Ellie Cannon supports the campaign: “As a GP, my working day will often include seeing someone for their cervical screening appointment. Cervical cancer is the only one of the five gynaecological cancers that has a screening programme in place, and we know that it saves thousands of lives each year. However, the appointment and actual test itself can sometimes prove to be very difficult for some people. Trans men, and people who are intersex or identify as non-binary face more obstacles than cis women. There is a wide spectrum of barriers affecting these communities.
“It’s my job to make sure the communication between myself and the patient is as open as possible, and I want them to know that we can take each step of the test at their own pace. The bottom line is that cervical screening needs to be more accessible to anyone with a cervix, and I’m proud to support The Eve Appeal in their aim to make this the case.”
Michelle O’Hara, who runs a trans specialist cervical screening clinic, 56 Dean Street, says: “Encouraging trans men, non-binary and intersex people with a cervix to have a smear is essential. As health care professionals, we continuously provide high standards and quality of care to our patients. It is important that patients know that they have complete control of their body, feel reassured and have the right say ‘stop’ at any time. A positive experience means that patients are more likely to engage in services in the future.”
Content provided by The Eve Appeal
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers – womb, ovarian, cervical, vulval and vaginal.

Published on Wed, 09 Mar 2022 15:06:26 GMT
Modified on Mon, 21 Mar 2022 10:20:51 GMT
Content provided by The Eve Appeal
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers – womb, ovarian, cervical, vulval and vaginal.

Published on Wed, 09 Mar 2022 12:30:35 GMT
Modified on Mon, 21 Mar 2022 10:30:50 GMT